Hypoxic-ischemic encephalopathy (HIE) is the most common cause of perinatal brain injury in full term infants – affecting up to three of every 1,000 births – and 40-60% of infants don’t make it past the age of 2 or suffer long-term neurological disabilities.
To combat this mortality rate and severity of brain injury, Linda Chalak, M.D., Division Chief of Neonatology at Children’s Medical Center Dallas, part of Children’s HealthSM, and Professor at UT Southwestern, is exploring new research and trials for HIE. The latest focal points include neuroprotective strategies and treatment modalities, such as modifications to cooling therapies and biomarkers for early HIE detection. Dr. Chalak summarizes the latest findings in Perinatal Asphyxia: Moving the Needle, an issue in “Clinics in Perinatology.”
“Babies with HIE need everything we can provide. The answers we reach today and tomorrow will enable neonatal teams across the country to meet that obligation," says Dr. Chalak.
Today: Current therapeutic hypothermia practices are still best
Therapeutic hypothermia (TH), also known as targeted temperature management, is widely practiced for moderate to severe HIE. Standard practice includes administration within 6 hours of life and cooling for 72 hours at a target core temperature of 33.5°C for body cooling (34.5°C for head cooling).
Multiple trials reviewed in the “Clinics in Perinatology” have explored changes to these practices, but so far none have led to better outcomes:
Cooling to a core temperature below 33.5°C and/or for longer than 72 hours yields no benefit and may increase mortality.
Administering TH to babies between 6 and 24 hours of life is likely to provide benefit, but not as likely or as much as TH administered within 6 hours.
Administering TH to preterm babies (33 to <36 weeks gestational age) does not decrease death or disability.
“These negative trials show that the longstanding approach to TH remains best,” says Dr. Chalak.
Near term: Data on therapeutic hypothermia in mild HIE
One practice that has not been standardized is whether teams should administer TH to babies with mild HIE. The COOL PRIME study, which is currently enrolling, will settle this question by tracking two-year outcomes for more than 300 babies across 18 sites: Nine that currently practice TH for mild HIE and nine that don’t.
This trial builds on the earlier PRIME trial, which demonstrated the long-term impact of mild HIE on neurodevelopment. In that trial, 16% of babies with mild HIE were diagnosed with a neurological disability by 22 months – and 40% had a development delay.
“We know that mild HIE harms babies, but we’ve never measured whether hypothermia is effective at reducing that harm. COOL PRIME will tell us,” Dr. Chalak says.
Long term: Improving care with biomarkers
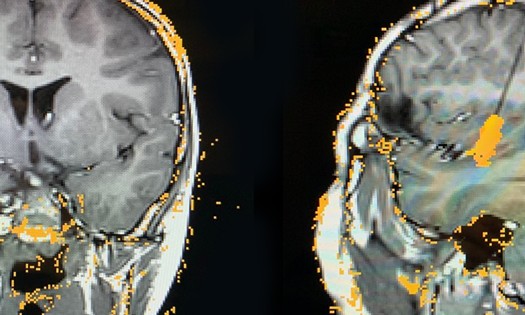
Diagnosing HIE depends on a clinical assessment of the newborn and is complicated by rapid changes in neurological indicators during the first hours of life. Ongoing research into biomarkers will give clinicians new ways to reach a diagnosis, assess severity and guide treatment.
EEG biomarkers can enhance HIE diagnosis and seizure management
Pediatric electroencephalography (EEG) is an important diagnostic tool because it reveals details and dangers the clinician cannot observe otherwise.
Abnormal EEG readings such as erratic signals and suppressed or reduced amplitude are reliable indicators of HIE.
Studies show that assessing HIE severity with EEG readings is more accurate than clinical assessment alone, which is prone to underestimation.
EEG can detect subclinical seizures and pre-seizure warning signs to help teams intervene promptly and preemptively.
Ideally, newborns with low Apgar scores, low oxygen levels or other factors associated with HIE should receive continuous monitoring with conventional EEG (cEEG), which provides more accurate readings than amplitude integrated EEG (aEEG). Continuous monitoring is not common today, but recent and upcoming advancements making cEEG more accessible and aEEG readings more accurate should help more centers adopt the practice.
Inflammatory biomarkers may lead to new treatments
Researchers have identified 14 cytokines and molecular proteins that proliferate in cord blood, postnatal blood, or both as part of the inflammatory cascade following hypoxic-ischemic insults. These biomarkers could lead to blood tests that help clinicians diagnose HIE without relying on observation alone.
Similarly, inter-alpha inhibitor proteins (IAIPs) show potential in not only diagnosing but also treating HIE. IAIPs are anti-inflammatory agents that appear in lower levels among babies with HIE.
“It’s possible that IAIP infusions could help reduce the inflammatory response and neurological harm,” Dr. Chalak says. “Therapeutic use of IAIPs hasn’t been tested in humans yet, but it was shown to reduce brain damage in a study of rodents exposed to HIE.”
Children’s Health’s longstanding expertise and innovation in neonatal care
Children’s Health has pioneered HIE research for decades, acting as the lead site for all foundational trials investigating therapeutic hypothermia, including the current COOL PRIME trial. Our Thrive Program at Children’s Medical Center Dallas combines comprehensive primary care for high-risk infants with follow-up for those infants participating in research, helping us achieve one of the highest follow-up rates in the nation.
In recognition of her work, Dr. Chalak was recently elected to the Association of American Physicians, of which less than 0.1% are pediatricians.
Learn more about innovations in neonatology at Children’s Health